Ultrasound
About Us
Welcome! This is the website for the Mount Sinai Emergency Ultrasound Division. It serves as an information resource for residents, fellows, medical students, and others seeking information about point-of-care ultrasound. The ultrasound division exists
There is a lot of information here, so please explore the site and send us feedback. To make things easier for new users we’ve condensed some of the highlights here:
Tutorials
We have put together multiple tutorials covering the FAST exam, the RUSH exam, cardiac ultrasound, obstetrics, pneumothorax assessment, and more. Instructions on using the S-Cath and M-Turbo.
For more academic posts, check out the ultrasound section of our FOAM page.
Rotation
We invite medical students and residents to apply for our ultrasound rotation and see the Manual that serves as our text.
Depending on the time of year we also offer ultrasound courses including our: ASM-I medical school course, Regional CME course, and NYC city-wide resuscitative ultrasound.
YouTube
You can see great POCUS videos on our POCUS4Peds YouTube channel and our SinaiEMultrasound YouTube Channel!
Recent Ultrasound Posts
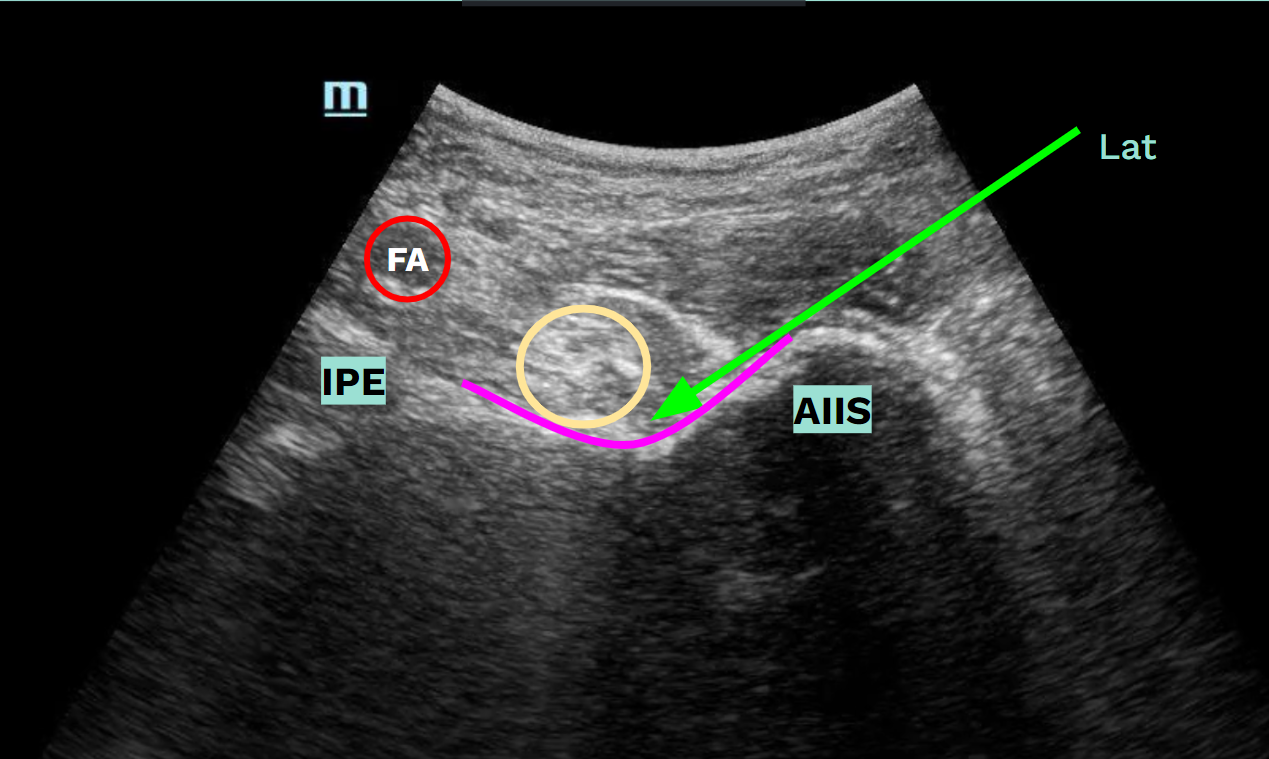
The PENG block is an effective, easy and safe way to provide analgesia to acute traumatic hip injuries
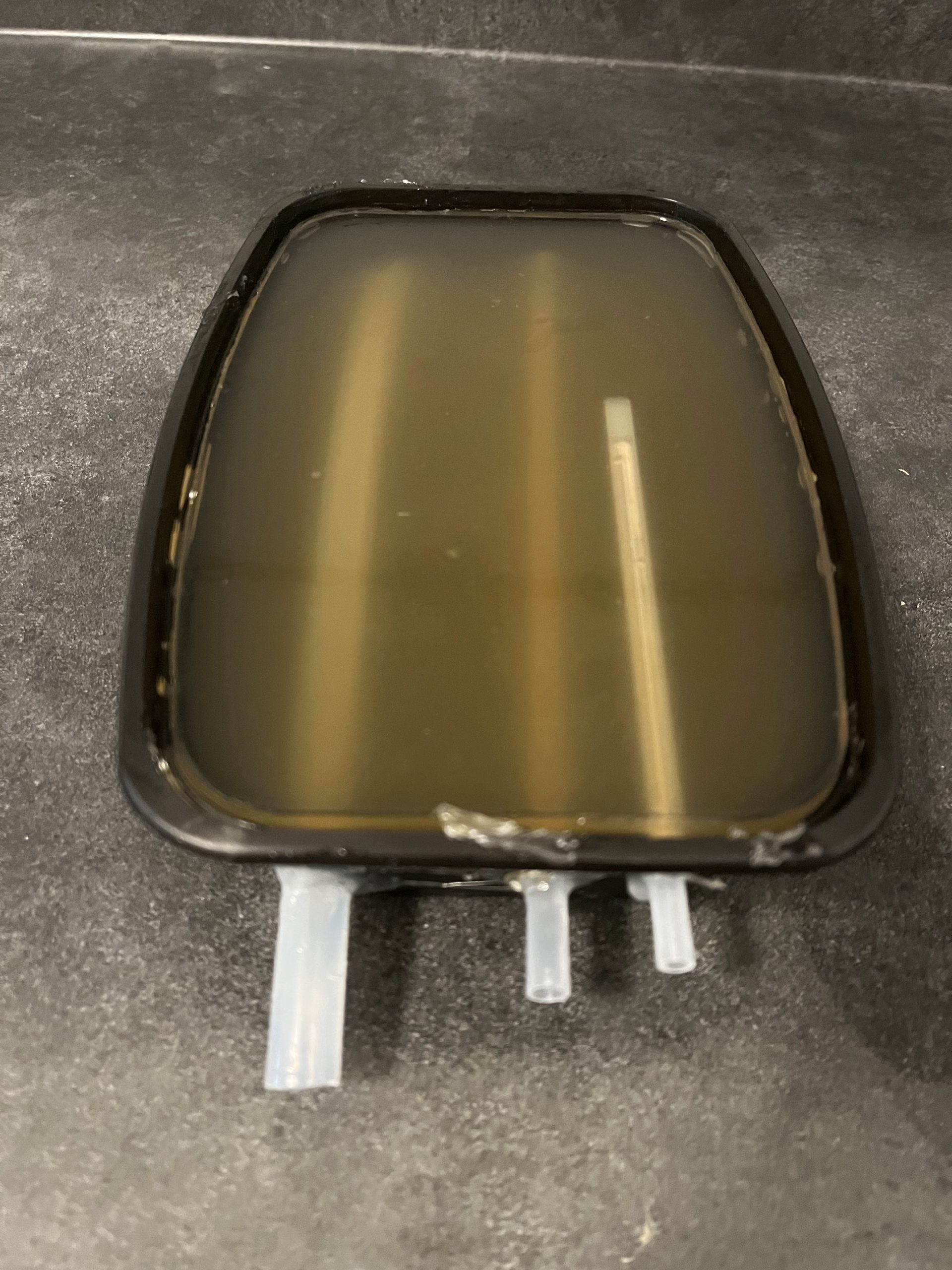
Step by step guide to build your own homemade ultrasound gelatin model for IV access. It’s simple, cheap and fast!

Ultrasound probe movements, the quest of the good vein, out-of-plane technique and in-plane technique of the ultrasound-guided intravenous line

